As financially hobbled hospitals struggle to survive amid the Covid-19 pandemic, some are turning to a Soviet-trained mathematician for help.
Eugene Litvak, a Harvard professor with a heavy Ukrainian accent, has emerged as a go-to guru for top health-care facilities, which collectively have lost billions since the outbreak.
The 70-year-old consultant and founder of the Newton, Mass.-based Institute for Healthcare Optimization (IHO) specializes in improving patient flow — from intake to discharge — and dealing with unexpected surges of critical cases, a problem that’s plagued hospitals for decades but spiked to crisis levels during the pandemic.
His algorithms and graphing models help predict overcrowding episodes and guide hospitals on how to respond when they do happen, exactly the kind of expertise currently in demand.
Litvak, who has worked with the Mayo Clinic, Massachusetts General Hospital and Johns Hopkins Medical Center, admits to being caught off guard by the intensity and magnitude of the coronavirus spread.
“But I was not surprised by the hospital reaction,” he said. “I knew they would cancel elective surgeries.”
These operations, which include heart surgeries, tumor removals and bone transplants, account for about half the revenue of hospitals nationwide. When they got cancelled in record numbers starting in March, hundreds of medical centers faced financial disaster.
Litvak has been advising them on how to handle coronavirus cases while resuming elective surgeries, a challenge that involves sorting through competing variables.
“Typically, we provide hospitals with multiple possible scenarios, each with associated quality of care improvements, costs and return on investment,” he said.
“Hospitals must systematically match their capacity — beds, staffing and resources — with the demand to create optimal capacity for elective surgery patients.”
The threat of a Covid resurgence means now is the time to act, according to Litvak.
“In many places the pandemic is waning and hospitals may have a narrow window to reduce their backlog of elective surgeries and strengthen their financial future for a second surge this fall,” he said.
Litvak is working with executives at Cedars-Sinai Medical Center in Los Angeles for an anticipated onslaught of new cases over the next few months.
The 886-bed facility needs to run more smoothly, according to its chief of surgery, Dr. Bruce Gewertz.
But he said Covid-19 offered “a tremendous opportunity to re-imagine the hospital’s surgery program.”
“My colleagues realized this was a great chance to do things in a more efficient way. We understand it will require behavioral and cultural changes, which are difficult in a large hospital. But I’ve never seen more unanimity on the part of surgical leadership that we have to do this.”
For now, Cedars-Sinai has decided against building a massive new wing for patients, which it had hoped would ease overcrowding, Gewertz said.
“At $3 million cost per bed, a new 1,000-bed tower would cost $3 billion,” he said. “That didn’t seem like a rational decision. We can no longer build our way out of this problem.”
Gewertz added that Litvak’s methods will “absolutely better prepare us for the next wave of the coronavirus.”
The consultant’s work has already produced results for Toronto’s largest hospital system, the University Health Networks.
Prior to the pandemic Litvak asked UHN’s surgical units to create eight categories of elective procedures and determine how long patients could safely wait for each operation, ranging from 45 minutes to 14 days.
His team “helped us to prepare for the flu and coronavirus,” said Dr. Shaf Keshavjee, UHN’s chief of surgery.
“They helped us to use our data to prepare our hospitals for other events, disasters and epidemics. Even if there comes a second surge, we are better prepared now to respond quickly and if cases creep up, we can watch and react in real time,” he said.
“Being more organized in our approach to surgery and recognizing the many forces influencing our ability to deliver care has helped us to modify our environment and change our practices.”
Litvak discovered long ago that clustering elective surgeries in the morning and early in the week proved disastrous when sudden rushes occurred in the ER. They led to ambulance diversions, intensive care unit overload and staff burnout — along with higher rates of medical errors and more preventable deaths.
So he focused on rethinking how to schedule surgeries in a way that accounted for all the elements involved.
“Different surgeries take different times to complete and require different lengths of recovery time in hospital beds, staffing and equipment,” he said. “Also, different surgeries have different financial margins. Some are more lucrative than others.”
He noted, “Without having the data to make the right decisions — balancing demand capacity and profit margins — [hospitals] are shooting in the dark.”
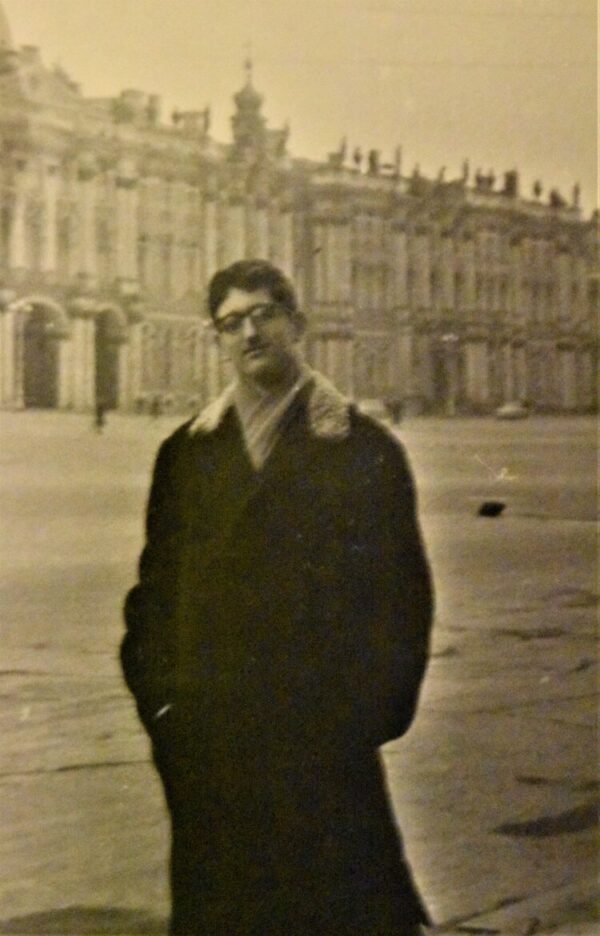
The emergence of Litvak comes after decades of personal struggles.
He was born in the ashes of bombed-out Kiev following World War II, with a family that had narrowly escaped execution and Jewish pogroms.
He got expelled from college in St. Petersburg for missing classes but went on to earn a Ph.D. in applied mathematics and publish ground-breaking research, co-authoring a paper with a Nobel Prize winner.
It took Litvak 10 years to emigrate from the USSR as a refusenik, during which he was hounded by KGB officers, who would not allow him to leave unless he agreed to spy on fellow scientists. He refused, so they stripped him of his academic position, and he delivered telegrams while his wife washed floors.
Eventually the couple and their parents emigrated with $150 in their pockets.
After arriving in the U.S. in 1988, Litvak became a postdoctoral fellow at Harvard, despite his limited English, and developed a new testing model for screening HIV in blood that was safer, less expensive and more accurate than the existing testing models. It was successfully adopted in several countries.
It was at Harvard where Litvak found his calling: trying to solve the many problems affecting American hospitals caused by overcrowding — rampant waste, uneven quality of care, spiraling costs — which, he discovered, could be reduced by controlling patient flow variability.
The stakes were huge. Between 25 and 33 percent of the $3.6 trillion spent on health care in the U.S. in 2018 was wasted on inefficiency, duplication and unnecessary treatments, studies have shown.
His ideas began to gain traction after a 2012 paper in the Journal of the American Medical Association estimated that if every U.S. hospital adopted Litvak’s methods, the U.S. health-care system would save between $120 billion and $150 billion annually.
“As a country, we are at this point really starving for improvements in care delivery that not only improve quality, but equally important, make health insurance more affordable,” said Dr. Arnold Milstein, a Stanford University professor and co-author of the study.
Litvak’s ideas are “the best near-term play for changing health-care delivery in a way that would meaningfully reduce spending and improve quality,” said Milstein, a leading researcher on the subject, to the Boston Globe in 2009.
Harvey Fineberg, who heads a committee on Covid-19 at the National Academies of Science, Engineering and Medicine, is also a fan of Litvak’s work.
“These relatively simple methods do require adjustments from hospitals and clinicians as well as a change in culture,” he said. “But these practices Litvak has championed have always been relevant and are even more salient during this pandemic.”
For now, Litvak is hoping that a new way of thinking emerges from the Covid outbreak.
“If there is any silver lining in this pandemic, it is that we would change our culture of delivering health-care services,” he said. “Perhaps this virus may make our hospitals truly more efficient and patient-centric.”